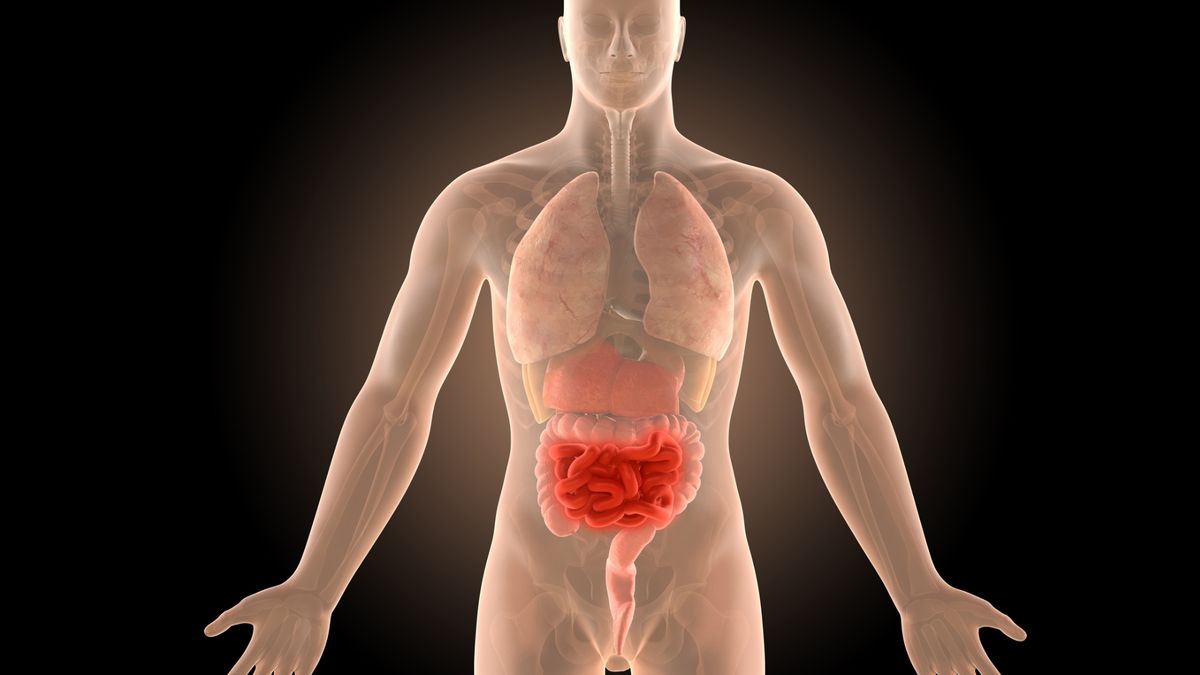
Crohn’s disease is a chronic inflammatory bowel disease (IBD) that affects the digestive tract, most commonly the small intestine and the beginning of the colon. It causes a wide range of symptoms including abdominal pain, diarrhea, fatigue, weight loss, and malnutrition. As a lifelong condition with no known cure, treatment for Crohn’s disease focuses on managing symptoms, reducing inflammation, and maintaining remission.
Effective treatment involves a combination of medications, dietary changes, lifestyle modifications, and sometimes surgery. This article explores the current treatment options available for Crohn’s disease and how they can help improve quality of life.
Goals of Crohn’s Disease Treatment
The primary goals in treating Crohn’s disease are:
- Reducing inflammation in the digestive tract
- Managing symptoms such as pain, diarrhea, and fatigue
- Preventing flare-ups and maintaining remission
- Healing damaged tissues in the intestines
- Improving overall well-being and nutrition
Because Crohn’s disease varies in severity and location from person to person, treatment plans are highly individualized.
Medications for Crohn’s Disease
Medications play a central role in controlling inflammation and managing symptoms.
1. Anti-Inflammatory Drugs
These are usually the first line of treatment, especially for mild to moderate Crohn’s disease.
- Aminosalicylates (e.g., mesalamine) help control inflammation in the intestines.
- Corticosteroids (e.g., prednisone) are used for short-term control during flare-ups due to their strong anti-inflammatory effects.
Note: Long-term use of corticosteroids is discouraged due to serious side effects, including bone loss, high blood pressure, and increased infection risk.
2. Immune System Suppressors
These medications target the immune response that causes inflammation.
- Azathioprine and 6-mercaptopurine (6-MP) are common immunosuppressants used to maintain remission.
- Methotrexate may be used when other drugs are not effective.
- Cyclosporine or Tacrolimus may be considered for severe cases.
3. Biologic Therapies
Biologics are advanced treatments designed to target specific pathways in the immune system.
- Anti-TNF agents (e.g., infliximab, adalimumab) help reduce inflammation by blocking tumor necrosis factor (TNF), a protein involved in inflammation.
- Integrin inhibitors (e.g., vedolizumab) prevent immune cells from entering inflamed tissue in the intestines.
- IL-12 and IL-23 inhibitors (e.g., ustekinumab) reduce inflammation by blocking certain immune pathways.
Biologics are often used in moderate to severe Crohn’s disease and have been highly effective in inducing and maintaining remission.
4. Antibiotics
Some patients benefit from antibiotics (e.g., metronidazole, ciprofloxacin), particularly if infections or abscesses are present.
Nutritional Therapy
Diet and nutrition play a critical role in managing Crohn’s disease. Malnutrition is common due to poor absorption, diarrhea, and reduced appetite.
Nutritional strategies include:
- Exclusive Enteral Nutrition (EEN): Liquid formulas used as the sole food source, often in children, to reduce inflammation.
- Low-residue or low-fiber diet: Helps reduce bowel volume and discomfort during flare-ups.
- Elimination diets: Identifying and avoiding trigger foods like dairy, gluten, spicy foods, or high-fat meals.
Supplements may be needed for deficiencies in iron, vitamin B12, vitamin D, calcium, and other nutrients.
Lifestyle Modifications
Lifestyle changes can help reduce the frequency and severity of flare-ups.
- Quit smoking: Smoking worsens Crohn’s disease and increases the need for surgery.
- Stress management: Stress does not cause Crohn’s, but it can trigger symptoms. Practices like meditation, yoga, and counseling can be beneficial.
- Exercise regularly: Moderate activity helps improve gut function, reduce stress, and maintain overall health.
- Stay hydrated: Chronic diarrhea increases the risk of dehydration.
Surgical Options
Surgery may be required when medications and other treatments fail to control symptoms or when complications arise.
Common reasons for surgery include:
- Intestinal blockages (strictures)
- Abscesses or fistulas
- Severe bleeding
- Perforation of the bowel
The most common surgical procedure is bowel resection, where the diseased portion of the intestine is removed. While surgery can provide relief, it does not cure the disease, and recurrence in other parts of the digestive tract is common.
Emerging Treatments and Research
Medical research is actively exploring new approaches to Crohn’s disease management, including:
- Stem cell therapy: Potential to “reset” the immune system.
- Fecal microbiota transplantation (FMT): Restores healthy gut bacteria.
- Personalized medicine: Genetic and microbiome profiling to tailor treatments to individuals.
- New biologics and small-molecule drugs: Offering more targeted immune modulation with fewer side effects.
Conclusion
Crohn’s disease is a complex, lifelong condition that requires a personalized and evolving treatment plan. While there is no cure, a combination of medications, nutrition, lifestyle adjustments, and surgical interventions can help manage the disease effectively and improve quality of life. Early diagnosis, close monitoring, and a collaborative approach between patient and healthcare team are essential for achieving long-term remission and minimizing complications. As research advances, new therapies continue to offer hope for better outcomes in the future.